After concussion: Helping students return to class
Several months ago, my son came home from school stating that his friend had been out of school for a week. The next week, he reported that his friend was still out of school. As an educator and parent, I became concerned. What had happened that was keeping this seventh grader out of school for such an extended time? I finally had to get nosy and ask and was surprised by the answer: he had suffered a concussion while playing in the yard.
According to the CDC, approximately three million children suffer traumatic brain injuries (TBIs) each year. 80-90% of these TBIs are considered mild, otherwise known as concussions.
What is a concussion? A concussion is a mild traumatic brain injury. It occurs when there is an outside forceful blow the head. 90% of concussions do not result in lost consciousness. Although a CT or MRI scan does not typically note differences in brain function, there are a variety of physical, emotional and behavioral changes after a concussion that may be temporary (1 to 2 weeks) or permanent.
I was able to speak to my son’s friend three weeks after the concussion and one week after the child had returned to school. She stated that her son was continuing to be extremely fatigued, found all math to be taxing and exhausting, and was having daily headaches. She was scared and concerned that maybe he shouldn’t have returned to school yet. And, she mentioned, she was frustrated that some of the students (and teachers?) felt like he was faking it. He looked fine after all.
This winter/spring, I have had the opportunity to attend several workshops about traumatic brain injury. One workshop was focused on concussions and the ways that the school can facilitate a smooth(er) transition for students returning to school after a concussion.
Almost all of this information can be downloaded from the CDC, along with extremely helpful handouts for teachers.
A child had a concussion and is coming back to school after being released by a doctor. Now what?
A team needs to be assembled to help in the transition back to school process. Members of this team should include:
- Student
- Parents
- Caregivers (coaches, babysitters, extended family)
- Doctors
- School nurse
- All school staff working with the student (teachers, specialists)
- SLP
- Administrator
- School counselor/psychologist
Everyone in the team should be aware that the student will likely exhibit new challenges for the school setting. These may include some or all of the following:
- Decreased attention span
- More difficulties learning new information
- Difficulties with memory
- Difficulties with initiating tasks
- Longer processing time required
- Difficulties with organization
- Difficulties with transitions
- Distorted memories
- Increased impulsivity
- Increased sensory sensitivities
- Headaches, nausea, dizziness
- Difficulty with emotional regulation
The team needs to draft a plan to help the student with classwork:
- Starting with minimal demands and slowly increase expectations over time
- Allowing extra time for work
- Modifying work to be shorter or less demanding
- Considering shortening the school day
- Allowing time in school to rest
- Limiting computer and screen exposure
- Creating a written or visual schedule for the day and assignments
- Enlisting a peer helper
- Giving frequent eye and brain breaks
The team also needs to determine a plan to help minimize the physical aspects of concussion, such as:
- Allowing alternative schedules to avoid PE and recess
- Providing rest time in or out of the classroom
- Allowing student time to visit the nurse to help with headaches or other physical symptoms
- Changing the classroom to decrease sensory overload
- Providing “quiet” areas or noise reducing headphones
Parents and teacher needs to be aware that cognitive rest is crucial following any kind of head injury. Some students may need to have a modified day or avoid school for a period of time to rest. During this time of cognitive rest, the student needs to attempt to avoid excessive activity that causes mental exertion. These include: screens (tablet, tv, computer), loud music, phone (texting, talking), reading, taxing academic mental tasks. These activities should be introduced back into the child’s life as tolerated and with intensity and duration increased slowly over the course of time. And if symptoms continue long term, the team needs to make decisions about implementing a 504, RTI, or IEP. That process is dictated by your district and/or state.
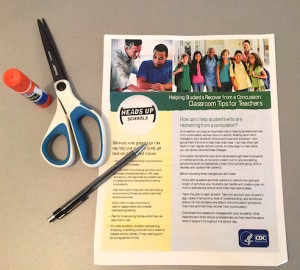 Grab the free downloads from the CDC here and pass them out to your team today!
Grab the free downloads from the CDC here and pass them out to your team today!
My son’s friend is doing well now thanks to a lot of rest and gradual transition back into school. Every year, parents, coaches, and educators are becoming more aware of what a concussion is and what to do after a concussion. In fact, twice a year when I register my son for soccer, I have to sign waivers that I understand the signs/symptoms of a concussion. My hope and prayer is that when next a student at my school returns to school after a concussion, the team (myself included) will be able to quickly and efficiently put a plan in place to help him/her be successful during the recovery period.
This post is part of a series on brain injuries. Read all the posts in this series here.
Reply below, super reader, and tell me your experiences with students in school following a concussion.